How to boost your immune system – Harvard Health
Tips to fight disease and strengthen immunity
 On the whole, your immune system does a remarkable job of defending you against disease-causing microorganisms. But sometimes it fails: A germ invades successfully and makes you sick. Is it possible to intervene in this process and make your immune system stronger? What if you improve your diet? Take certain vitamins or herbal preparations? Make other lifestyle changes in the hope of producing a near-perfect immune response?
On the whole, your immune system does a remarkable job of defending you against disease-causing microorganisms. But sometimes it fails: A germ invades successfully and makes you sick. Is it possible to intervene in this process and make your immune system stronger? What if you improve your diet? Take certain vitamins or herbal preparations? Make other lifestyle changes in the hope of producing a near-perfect immune response?
What can you do?
The idea of boosting your immunity is enticing, but the ability to do so has proved elusive for several reasons. The immune system is precisely that — a system, not a single entity. To function well, it requires balance and harmony. There is still much that researchers don’t know about the intricacies and interconnectedness of the immune response. For now, there are no scientifically proven direct links between lifestyle and enhanced immune function.
But that doesn’t mean the effects of lifestyle on the immune system aren’t intriguing and shouldn’t be studied. Researchers are exploring the effects of diet, exercise, age, psychological stress, and other factors on the immune response, both in animals and in humans. In the meantime, general healthy-living strategies are a good way to start giving your immune system the upper hand.
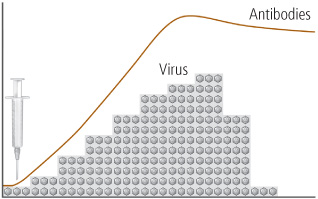
Immunity in action. A healthy immune system can defeat invading pathogens as shown above, where two bacteria that cause gonorrhea are no match for the large phagocyte, called a neutrophil, that engulfs and kills them (see arrows).
Photos courtesy of Michael N. Starnbach, Ph.D., Harvard Medical School
Adopt healthy-living strategies
Your first line of defense is to choose a healthy lifestyle. Following general good-health guidelines is the single best step you can take toward keeping your immune system strong and healthy. Every part of your body, including your immune system, functions better when protected from environmental assaults and bolstered by healthy-living strategies such as these:
- Don’t smoke.
- Eat a diet high in fruits, vegetables, and whole grains, and low in saturated fat.
- Exercise regularly.
- Maintain a healthy weight.
- Control your blood pressure.
- If you drink alcohol, drink only in moderation.
- Get adequate sleep.
- Take steps to avoid infection, such as washing your hands frequently and cooking meats thoroughly.
- Get regular medical screening tests for people in your age group and risk category.
Be skeptical
Many products on store shelves claim to boost or support immunity. But the concept of boosting immunity actually makes little sense scientifically. In fact, boosting the number of cells in your body — immune cells or others — is not necessarily a good thing. For example, athletes who engage in “blood doping” — pumping blood into their systems to boost their number of blood cells and enhance their performance — run the risk of strokes.
Attempting to boost the cells of the immune system is especially complicated because there are so many different kinds of cells in the immune system that respond to so many different microbes in so many ways. Which cells should you boost, and to what number? So far, scientists do not know the answer. What is known is that the body is continually generating immune cells. Certainly it produces many more lymphocytes than it can possibly use. The extra cells remove themselves through a natural process of cell death called apoptosis — some before they see any action, some after the battle is won. No one knows how many cells or what the best mix of cells the immune system needs to function at its optimum level.
Get your copy of Starting to Exercise
What can improve your mood, boost your ability to fend off infection, and lower your risk for heart disease, diabetes, high blood pressure, and colon cancer? The answer is regular exercise. It may seem too good to be true, but it’s not. Hundreds of studies demonstrate that exercise helps you feel better and live longer. This report answers many important questions about physical activity. It will also help guide you through starting and maintaining an exercise program that suits your abilities and lifestyle.
Age and immunity
The aging process somehow leads to a reduction of immune response capability, which in turn contributes to more infections, more inflammatory diseases, and more cancer. As life expectancy in developed countries has increased, so too has the incidence of age-related conditions. Happily, investigation into the aging process can benefit us all — no matter what our age.
While some people age healthily, the conclusion of many studies is that, compared with younger people, the elderly are more likely to contract infectious diseases and, even more importantly, more likely to die from them. Respiratory infections, influenza, and particularly pneumonia are a leading cause of death in people over 65 worldwide. No one knows for sure why this happens, but some scientists observe that this increased risk correlates with a decrease in T cells, possibly from the thymus atrophying with age and producing fewer T cells to fight off infection. Thymus function declines beginning at age 1; whether this decrease in thymus function explains the drop in T cells or whether other changes play a role is not fully understood. Others are interested in whether the bone marrow becomes less efficient at producing the stem cells that give rise to the cells of the immune system.
A reduction in immune response to infections has been demonstrated by older people’s response to vaccines. For example, studies of influenza vaccines have shown that for people over age 65, the vaccine is much less effective compared to healthy children (over age 2). But despite the reduction in efficacy, vaccinations for influenza and S. pneumoniae have significantly lowered the rates of sickness and death in older people when compared with no vaccination.
There appears to be a connection between nutrition and immunity in the elderly. A form of malnutrition that is surprisingly common even in affluent countries is known as “micronutrient malnutrition.” Micronutrient malnutrition, in which a person is deficient in some essential vitamins and trace minerals that are obtained from or supplemented by diet, can be common in the elderly. Older people tend to eat less and often have less variety in their diets. One important question is whether dietary supplements may help older people maintain a healthier immune system. Older people should discuss this question with a physician who is well versed in geriatric nutrition, because while some dietary supplementation may be beneficial for older people, even small changes can have serious repercussions in this age group.
What about diet?
Like any fighting force, the immune system army marches on its stomach. Healthy immune system warriors need good, regular nourishment. Scientists have long recognized that people who live in poverty and are malnourished are more vulnerable to infectious diseases. Whether the increased rate of disease is caused
There is some evidence that various micronutrient deficiencies — for example, deficiencies of zinc, selenium, iron, copper, folic acid, and vitamins A, B6, C, and E — alter immune responses in animals, as measured in the test tube. However, the impact of these immune system changes on the health of animals is less clear, and the effect of similar deficiencies on the human immune response has yet to be assessed. But the research at this stage is promising, at least for some of the micronutrients.
So what can you do? If you suspect your diet is not providing you with all your micronutrient needs — maybe you don’t like vegetables or you choose white bread over whole grains — taking a daily multivitamin and mineral supplement brings health benefits of many types, beyond any possibly beneficial effects on the immune system. Taking megadoses of a single vitamin does not. More is not necessarily better. Researchers are investigating the immune boosting potential of a number of different nutrients.
Herbs and other supplements
Walk into a store, and you will find bottles of pills and herbal preparations that claim to “support immunity” or otherwise boost the health of your immune system. Although some preparations have been found to alter some components of immune function, thus far there is no evidence that they actually bolster immunity to the point where you are better protected against infection and disease. Demonstrating whether an herb — or any substance, for that matter — can enhance immunity is, as yet, a highly complicated matter. Scientists don’t know, for example, whether an herb that seems to raise the levels of antibodies in the blood is actually doing anything beneficial for overall immunity.
The stress connection
Modern medicine, which once treated the connection between emotions and physical health with skepticism, has come to appreciate the closely linked relationship of mind and body. A wide variety of maladies, including stomach upset, hives, and even heart disease, are linked to the effects of emotional stress. But although the relationship between stress and immune function is being studied by a number of different types of scientists, so far it is not a major area of research for immunologists.
Studying the relationship between stress and the immune system presents difficult challenges. For one thing, stress is difficult to define. What may appear to be a stressful situation for one person is not for another. When people are exposed to situations they regard as stressful, it is difficult for them to measure how much stress they feel, and difficult for the scientist to know if a person’s subjective impression of the amount of stress is accurate. The scientist can only measure things that may reflect stress, such as the number of times the heart beats each minute, but such measures also may reflect other factors.
Most scientists studying the relationship of stress and immune function, however, do not study a sudden, short-lived stressor; rather, they try to study more constant and frequent stressors known as chronic stress, such as that caused by relationships with family, friends, and co-workers, or sustained challenges to perform well at one’s work. Some scientists are investigating whether ongoing stress takes a toll on the immune system.
But it is hard to perform what scientists call “controlled experiments” in human beings. In a controlled experiment, the scientist can change one and only one factor, such as the amount of a particular chemical, and then measure the effect of that change on some other measurable phenomenon, such as the amount of antibodies produced by a particular type of immune system cell when it is exposed to the chemical. In a living animal, and especially in a human being, that kind of control is just not possible, since there are so many other things happening to the animal or person at the time that measurements are being taken.
Despite these inevitable difficulties in measuring the relationship of stress to immunity, scientists who repeat the same experiment many times with many different animals or human beings, and who get the same result most of the time, hope that they can draw reasonable conclusions.
Get your copy of Vitamins and Minerals

About half of all Americans routinely take dietary supplements. The most common ones are multivitamin and multimineral supplements. This report explains the evidence behind the benefits and safety profiles of various vitamins and minerals. It also includes the recommended minimum and maximum amounts you should consume, as well as good food sources of each.
Does being cold make you sick?
Almost every mother has said it: “Wear a jacket or you’ll catch a cold!” Is she right? So far, researchers who are studying this question think that normal exposure to moderate cold doesn’t increase your susceptibility to infection. Most health experts agree that the reason winter is “cold and flu season” is not that people are cold, but that they spend more time indoors, in closer contact with other people who can pass on their germs.
But researchers remain interested in this question in different populations. Some experiments with mice suggest that cold exposure might reduce the ability to cope with infection. But what about humans? Scientists have dunked people in cold water and made others sit nude in subfreezing temperatures. They’ve studied people who lived in Antarctica and those on expeditions in the Canadian Rockies. The results have been mixed. For example, researchers documented an increase in upper respiratory infections in competitive cross-country skiers who exercise vigorously in the cold, but whether these infections are due to the cold or other factors — such as the intense exercise or the dryness of the air — is not known.
A group of Canadian researchers that has reviewed hundreds of medical studies on the subject and conducted some of its own research concludes that there’s no need to worry about moderate cold exposure — it has no detrimental effect on the human immune system. Should you bundle up when it’s cold outside? The answer is “yes” if you’re uncomfortable, or if you’re going to be outdoors for an extended period where such problems as frostbite and hypothermia are a risk. But don’t worry about immunity.
Exercise: Good or bad for immunity?
Regular exercise is one of the pillars of healthy living. It improves cardiovascular health, lowers blood pressure, helps control body weight, and protects against a variety of diseases. But does it help maintain a healthy immune system? Just like a healthy diet, exercise can contribute to general good health and therefore to a healthy immune system. It may contribute even more directly by promoting good circulation, which allows the cells and substances of the immune system to move through the body freely and do their job efficiently.
Some scientists are trying to take the next step to determine whether exercise directly affects a person’s susceptibility to infection. For example, some researchers are looking at whether extreme amounts of intensive exercise can cause athletes to get sick more often or somehow impairs their immune function. To do this sort of research, exercise scientists typically ask athletes to exercise intensively; the scientists test their blood and urine before and after the exercise to detect any changes in immune system components. While some changes have been recorded, immunologists do not yet know what these changes mean in terms of human immune response.
But these subjects are elite athletes undergoing intense physical exertion. What about moderate exercise for average people? Does it help keep the immune system healthy? For now, even though a direct beneficial link hasn’t been established, it’s reasonable to consider moderate regular exercise to be a beneficial arrow in the quiver of healthy living, a potentially important means for keeping your immune system healthy along with the rest of your body.
One approach that could help researchers get more complete answers about whether lifestyle factors such as exercise help improve immunity takes advantage of the sequencing of the human genome. This opportunity for research based on updated biomedical technology can be employed to give a more complete answer to this and similar questions about the immune system. For example, microarrays or “gene chips” based on the human genome allow scientists to look simultaneously at how thousands of gene sequences are turned on or off in response to specific physiological conditions — for example, blood cells from athletes before and after exercise. Researchers hope to use these tools to analyze patterns in order to better understand how the many pathways involved act at once.
Updated: June 15, 2016
Originally published: September 2014
